KINGSTON, R.I., Jan. 10, 2018—Imagine a onesie for newborns that can treat jaundice, a water bottle that prevents dehydration in the elderly or socks that keep the blood flowing in people with diabetes.
University of Rhode Island biomedical engineering students have created these projects and more as part of a cutting-edge class about a field that is revolutionizing the business market and healthcare industry: wearable technology.
“The Wearable Internet of Things,” taught by Kunal Mankodiya, an assistant professor of biomedical engineering at URI and director of URI’s Wearable Biosensing Laboratory, is sparking projects that are creative, innovative and, in many cases, commercially viable. Joshua Gyllinsky, a graduate student researcher, is also helping to teach the class.
“Our students are designing incredible wearable technologies,” says Mankodiya. “I’m privileged to guide them along and help them flourish.”

Wearables, as they’re known among techies, are essentially electronics that can be worn on the body, as clothing or an accessory. They are embedded with sensors, electronics and software that collect data and communicate it to users, patients and caregivers.
The benefits are profound. Patients can remain at home while a doctor monitors their health from afar, measuring through iPad-like devices medical symptoms such as heart rate, respiration rate, activity and even posture. There are also psychological benefits: patents and their families are more involved in the care.
The URI students worked on their projects for months, presenting them in mid-December to faculty and other students. Most of the students are biomedical engineering majors, while several are computer and electrical engineers.
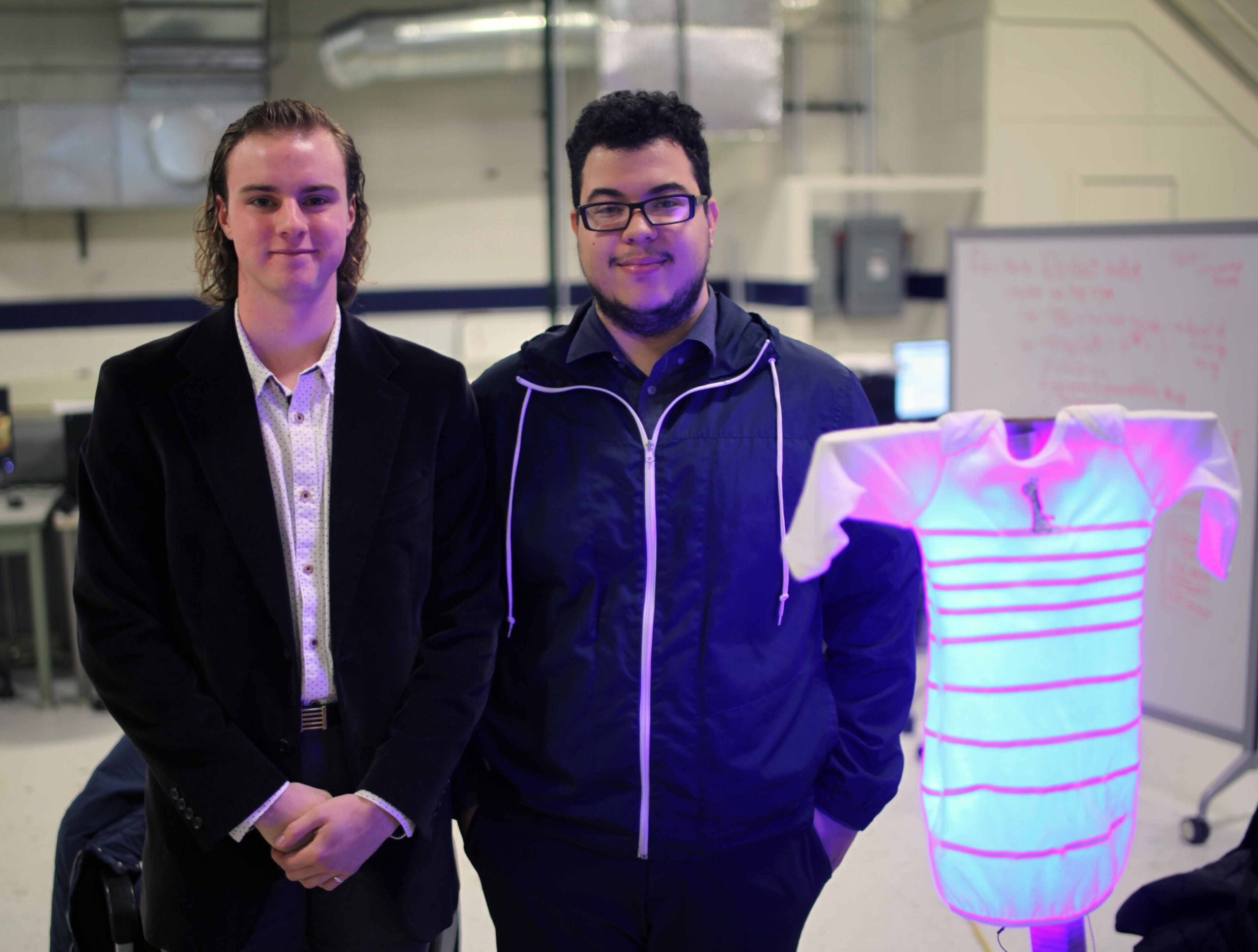
Joshua Harper, of Gray, Maine, and James Baez, of Providence, created a smart onesie to treat newborns with jaundice. The students were inspired by a friend, a URI nursing student, seeking better treatment for the condition, which is common in preterm babies.
The two methods used now have drawbacks, says Harper.
“We think our project fills the gap where other treatments have fallen short,” says Harper. “We’re excited about its potential.”
Infant jaundice is a yellowing of the skin and eyes caused by too much bilirubin, a yellow-colored pigment of red blood cells. An underdeveloped liver is often the culprit.
There are two treatments that work on the principle that light therapy breaks down bilirubin, Harper says.
The photo-therapy box is the most common treatment, but it’s far from perfect. The infant cannot be held, missing out on skin-to-skin contact with a parent. And eye damage is a risk if the baby pulls off the required protective glasses.
Swathing the baby in a Biliblanket is another option. Home treatment is possible, the baby can he held, and the risk of eye damage is eliminated, but the blanket only covers the baby’s torso, requiring longer treatment time.
The URI students’ J-Suit, or Jaundice Suit, offers the “positive aspects of the Biliblanket while also allowing the infants entire body to be exposed to the photo-therapy,” says Harper. “It covers the arms and legs, as well as the torso.”
The J-Suit contains hundreds of Light Emitting Diodes, or LEDs. The clothing is designed with wireless connectivity that allows a smartphone to control the LEDs remotely and collect data for parents and doctors to track the baby’s progress.
Other projects also showed strong potential for the business market.
Ryan Ivone, of Coventry, and Matt Cohen, of Pawtucket, created a smart water bottle that helps prevent dehydration in older people. Dehydration is a serious problem among older adults, especially those in nursing homes and assisted living facilities. In fact, many medications prescribed for the elderly, including anti-depressants and blood pressure medicine, can lead to dehydration, which can cause walking difficulties, dizziness and confusion.
“Normally, we use thirst as a signal that tells us when and how much to drink,” says Ivone. “As we age, this signal becomes weaker, and many times older people don’t actually feel thirsty even though they haven’t had anything to drink for a long time and need fluids. Many older people also have memory loss issues and can’t remember when they last had fluids.”
Keeping track of how much a patient drinks is time consuming for caregivers. Enter the smart water bottle, which sits on a computerized stand in the patient’s room and communicates wirelessly to the hospital’s Internet system, measuring how much water is, or is not, consumed in a designated period of time. The same method can be applied at home, where patients, or caregivers, could use WiFi or Bluetooth to track fluid consumption.
Helping people with diabetes and blood-circulation problems kept Gregory D’Ambrosca, of West Warwick, and Aaron Gilmore, of Barrington, busy in the class. Lack of blood flow can lead to painful ulcers, especially in the feet and calves. One way to stimulate blood flow is by being active, but many older people find it burdensome to take walks regularly. Massaging the feet is a solution.
“We created wearable socks that give foot massages to patients who are unable to move much,” says Gilmore. “A microcontroller mounted to the sock is paired with an accelerometer and three vibration actuators which are similar to the ones found in cell phones. When the accelerometer detects no motion, vibration actuators activate in a downward motion. This mimics a massage by pushing blood downward toward the toes to stimulate blood flow.”
Mary Ellen Sweeney, of Plainfield, Conn., Tian Chen, and Scott Barlow created a “Bionic Hand” in a skeleton design that helps stroke patients regain movement in their fingers. The project, also known as the “Exoskeleton Hand,” has two hands—one for the patient, the other for the caregiver, who can lead exercises from another location.
“What makes the project special is that patients can stay in their homes,” says Sweeney. “It’s convenient and less costly. We want to continue the project and maybe possibly get a patent one day.”
Nathan Ankomah-Mensah, of Pawtucket, Sawyer Nichols, of Portsmouth, and Zachary Silveira came up with a clever way to measure exposure to harmful ultraviolet rays in real time through a mobile device. Using UV sensors and a microcontroller board to detect the UV index, the glasses allow users to see how much exposure they’re getting so they can get out of the sun or apply more sunscreen. Nichols also envisions an upgrade that would alert users on their cell phones if their sun exposure is reaching dangerous levels.
“The class gave us an exciting chance to bring to life our own innovations,” says Nichols. “What makes Professor Mankodiya’s course so unique is the entrepreneurial approach. It’s an awesome opportunity for engineering undergraduates, with applications to the world.”